Ventral Hernia
What is a ventral hernia?
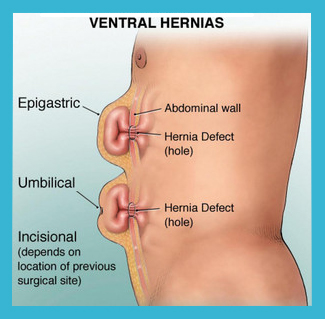
A ventral hernia arises in the front of the abdomen, where the abdominal muscles have weakened, resulting in a bulge or a tear. In the same way that an inner tube pushes through a damaged tire, the inner lining of the abdomen pushes through the weakened area of the abdominal wall to form a balloon-like sac. This can allow a loop of intestine or other abdominal contents to push into the sac. If the abdominal contents get stuck within the sac, they can become trapped or “incarcerated.” This could lead to potentially serious problems that might require emergency surgery. A hernia does not get better over time, nor will it go away by itself.
How do I know if I have a ventral hernia?
A hernia is usually recognized as a bulge under your skin. Occasionally, it causes no discomfort at all, but you may feel pain when you lift heavy objects, cough, and strain during urination or bowel movements or with prolonged standing or sitting. The discomfort may be sharp or a dull ache that gets worse towards the end of the day. Any continuous or severe discomfort, redness, nausea or vomiting associated with the bulge are signs that the hernia may be entrapped or strangulated. These symptoms are cause for concern and immediate contact of a surgeon is recommended.
What are the advantages of a laparoscopic repair?
Results may vary depending on the type of procedure and each patient’s overall condition. Common advantages may include:
- Less post-operative pain
- Tiny skin incisions
- Shortened hospital stay
- Quicker return to normal activity
OPEN HERNIA REPAIRS
Not all hernias should be performed laparoscopically. Sometimes the strongest hernia repair comes from an open surgery method where some of the abdominal wall muscles are freed up from attachments and approximated over the hernia defect and a mesh is often overlaid for additional repair strength.
We repair hernias in both open and laparoscopic methods, both with and without a mesh, both with and without muscle separation. Operating on thousands of obese patients over the last 13 years has also taught us how to safely perform laparoscopic procedures on patients who can often be more challenging.
What Should I Expect After Surgery?
Patients are encouraged to engage in light activity while at home after surgery. Post-operative discomfort is mild to moderate, and pain medication is given. Most patients are able to get back to their normal activities in a short period of time.
GERD / HIATAL HERNIA / ACID REFLUX
SURGERY FOR GASTRIC ACID REFLUX (GERD)
If you suffer from “heartburn” you may need laparoscopic anti-reflux surgery to treat this condition, technically referred to as Gastro-Esophageal Reflux Disease or GERD.
What is GERD (Gastro-Esophageal Reflux Disease)?
Stomach acids reflux or “back up” from the stomach into the esophagus. This causes a burning sensation in the area in between your ribs or just below your neck. The feeling may radiate through the chest and into the throat and neck. This is also known as heartburn. Many adults in the United States experience this uncomfortable, burning sensation at least once a month. Other symptoms may also include vomiting, difficulty swallowing and chronic coughing or wheezing.
What causes GERD?
When you eat, food travels from your mouth to your stomach through a tube called the esophagus. At the lower end of the esophagus is a small ring of muscle that acts like a one-way valve, allowing food to pass through into the stomach. Normally, this valve closes immediately after swallowing to prevent back up of stomach juices, which have a high acid content, into the esophagus. GERD occurs when this valve does not function properly allowing acid to flow back and burn the lower esophagus. This irritates and inflames the esophagus, causing heartburn and eventually may damage the esophagus, and increase the likelihood of esophageal cancer.
Some people are born with a naturally weak sphincter valve. For others, however, fatty and spicy foods, certain types of medication, tight clothing, smoking, drinking alcohol, vigorous exercise, bending over or lying down may cause this valve to relax, causing reflux.
What is a hiatal hernia?
A hiatal hernia is a defect in the Esophageal Sphincter, which allows stomach acid to reflux up into the esophagus. Fixing this hernia is often required to prevent stomach acid from refluxing upward, and get relief of GERD.
How is GERD treated?
1. Lifestyle changes – In many cases, changing diet, losing weight, reducing or eliminating smoking and alcohol consumption, and altering eating and sleeping patterns can help.
2. Medication therapy – If symptoms still persist, drug therapy may be required. Antacids neutralize stomach acids and over-the-counter medications reduce the amount of stomach acid produced. Both may be effective in relieving symptoms. Prescription drugs may be more effective in healing irritation of the esophagus and relieving symptoms.
3. Surgery – Patients who do not respond well to lifestyle changes or medications or those who continually require medications to control their symptoms, will have to live with their condition or may undergo a surgical procedure. Surgery is very effective in treating GERD.
How is Laparoscopic anti-reflux surgery performed?
Laparoscopic anti-reflux surgery (commonly referred to as Laparoscopic Nissen Fundoplication) involves reinforcing the “valve” between the esophagus and the stomach by wrapping the upper portion of the stomach around the lowest portion of the esophagus – much the way a bun wraps around a hot dog. In a laparoscopic procedure, Dr. Mehta uses small 1/4 inch incisions to enter the abdomen through tube-like laparoscopic instruments & a tiny video camera. The procedure is performed in this manner in about 45 minutes.
The advantage of the laparoscopic approach is that it usually provides:
- Reduced postoperative pain
- Shorter hospital stay
- A faster return to work
- Improved cosmetic result
- This procedure is usually performed as same day surgery where patients go home the same evening
What should I expect after surgery?
- Post-operative pain is generally mild although some patients may require prescription pain medication.
- Anti-reflux medication is usually not required after surgery.
- Diet after surgery begins with liquids followed by gradual advance to solid foods.
- You will probably be able to get back to your normal activities within a short amount of time. These activities include showering, driving, walking up stairs, lifting, working and engaging in sexual intercourse.
Are there side effects to this operation?
Studies have shown that the vast majority of patients who undergo the procedure are either symptom-free or have significant improvement in their GERD symptoms.
Long-term side effects to this procedure are generally uncommon.
Some patients develop temporary difficulty swallowing immediately after the operation. This usually resolves within one to three months after surgery.
- Occasionally, patients may require a procedure to stretch the esophagus (endoscopicdilation) or rarely re-operation.
- The ability to belch and or vomit may be limited following this procedure. Some patients report stomach bloating.
- Rarely, some patients have no improvement in their symptoms.
If you have chronic acid reflux (GERD), feel free to ask Dr. Mehta about your options.
Have questions about this procedure? Ask us now:
We accept all major insurances if you have appropriate benefits, offer financing, and can email you our specials, for those who choose to self-pay.
